Exercise Physiology
Exercise physiology is managed jointly by the brain and the cardiovascular system
Cardiovascular responsibilities during exercise
The cardiovascular system has distinct tasks to accomplish during exercise that are outside its routine function.
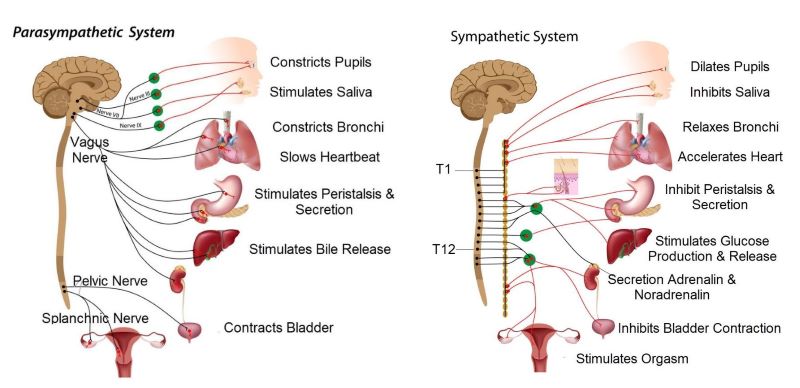
Exercise requires collaboration between the cardiovascular and nervous system, illustration by SciePro, Shutterstock.com
First, the cardiovascular system must deliver extra oxygen to skeletal muscle to support a high rate of metabolism. An elevated metabolic rate is needed at the skeletal muscles to make enough ATP for contractile activity.
Ample blood flow to skeletal muscles is required to wash out metabolic end products like lactic acid and carbon dioxide. While supplying skeletal muscles with extra blood flow, the cardiovascular system must keep blood pressure steady throughout the body.
The lungs, the kidneys, and the brain especially require a steady blood pressure to maintain their function during exercise. So, how does the cardiovascular system manage its responsibilities during the stress of exercise?
The answer is that the cardiovascular system depends upon the nervous system to help it out.
Increased lung ventilation during exercise
For the cardiovascular system to deliver more oxygen to the body, lung ventilation must increase during exercise. The rate of lung ventilation is controlled by the respiratory centers in the medulla and pons of the brainstem.
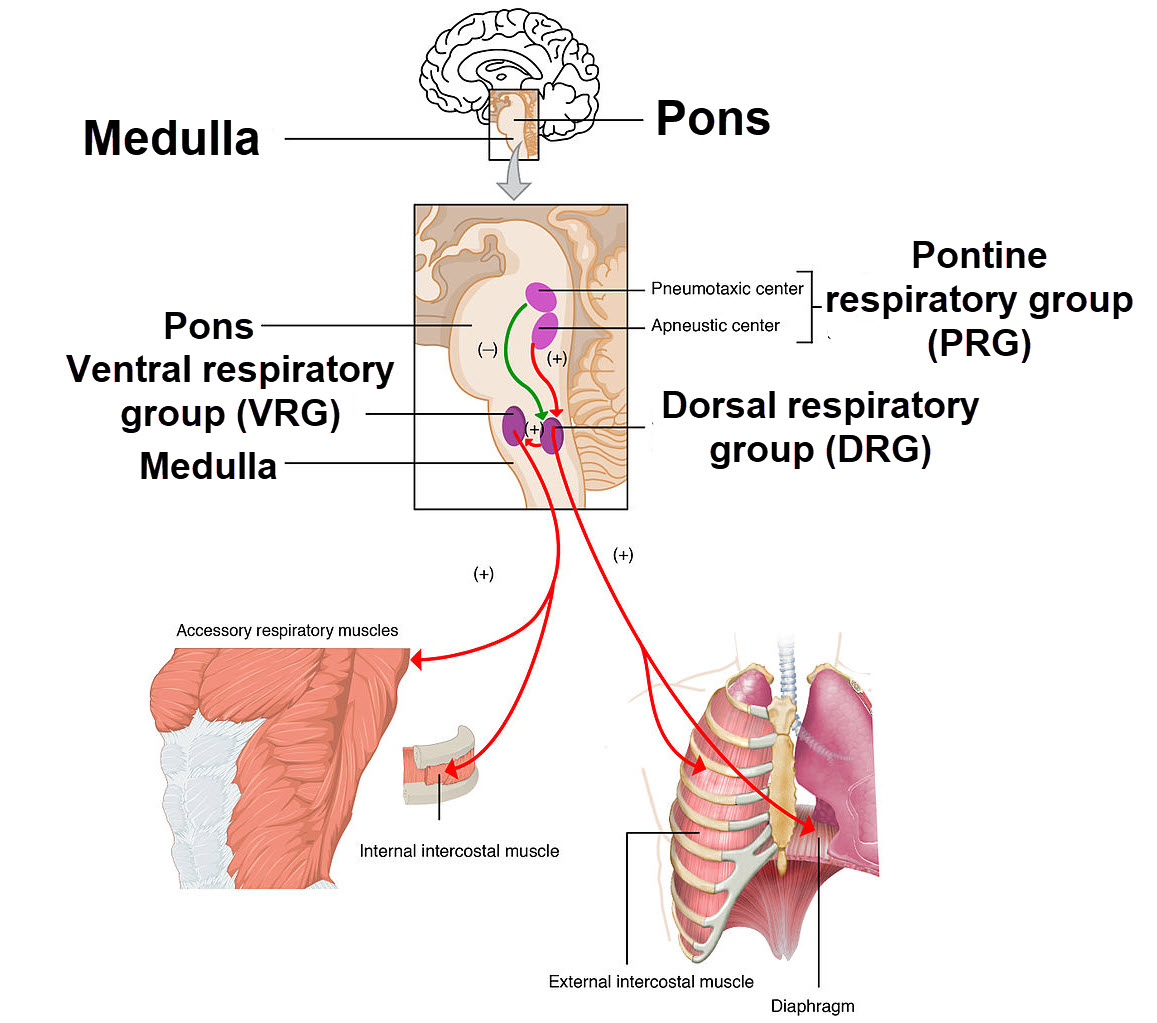
Four brainstem nuclei control rhymical inhalation by the lungs, OpenStax College, Wiki Media Commons
Input to the respiratory centers includes signals from peripheral and central chemoreceptors, from pulmonary stretch receptors, from the cerebral cortex, and from the hypothalamus.
During exercise, the chemoreceptors signal an acidic blood pH caused by the addition of metabolic carbon dioxide. The respiratory centers respond to this pH change by increasing their rate of signaling, which increases the lung ventilation rate.
Increased lung ventilation and heart rate at onset of exercise
For decades, exercise physiologists were puzzled by an increase in lung ventilation and heart rate at the very onset of exercise, prior to activation of blood chemoreceptors. These exercise-related changes occurred before there was increased metabolism requiring clearance of carbon dioxide and before there was a need for increased cardiac output.
It is now believed that a brain process named central command anticipates the physiologic requirements of exercise. Central command is guided by memory of previous experience. It does not wait for normal physiologic sensors to quantify the intensity of the exercise before it begins supplying elevated blood flow and increased ventilation.

Memory of previous exercise adapts’ cardiac output and lung ventilation rate to the individual, , jorgen mcleman, Shutterstoc.com
When a person exercises regularly, central command initiates an appropriate increase in respiratory rate and heart rate for that individual. What is judged appropriate depends upon memory of earlier periods of exercise.
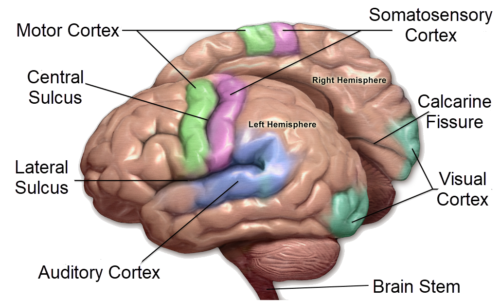
Neuroscientists determined that central command is a coordinated process of multiple parts of the brain.
Motor cortex signaling to respiratory centers
The unconscious process of exercise central command was shown to include, among other brain activity, motor cortex signaling to the respirator centers of the brain stem.
During exercise, central command borrows the motor pathway for conscious control of respiratory muscles. Motor neurons of the cerebral cortex, activated by central command, increase the activity of the brain stem respiratory pacemaker cells.
In response to somatic motor activity, the respiratory rhythm generators signal an increase the rate of contraction of the accessory respiratory muscles, the external and internal and external intercostal muscles, and the diaphragm.
Autonomic stimulation of cardiac output and bronchial dilation
Exercise’s central command also increases cardiac output and bronchial dilation. It does this by downregulating parasympathetic activity. With the decrease in parasympathetic activity, cardiac output is improved by a faster heart rate and greater strength of cardiac muscle contraction. Removal of parasympathetic activity also leads to dilation of the bronchi, which improves entry of air during inhalation.
As parasympathetic activity decreases, sympathetic neural activity increases. Brain stem nuclei reciprocally regulate the two divisions of the autonomic nervous system as illustrated above. The increase in sympathetic activity has an additional positive effect on cardiac output.
In summary, during exercise the autonomic nervous system’s effect on cardiac output and bronchial dilation is a result of both the withdrawal of parasympathetic activity and the increase in sympathetic activity.
Stabilization of blood pressure during exercise
Stabilization of blood pressure during exercise is necessary for perfusion of vital organs. Exercising muscles receive a large portion of the cardiac output. Elevated metabolites maintain dilation of the skeletal muscle blood vessels.
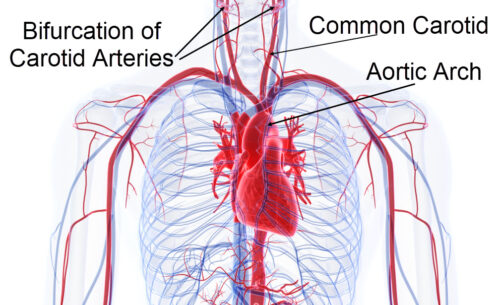
Stabilization of cardiovascular blood pressure during exercise again requires help of the autonomic nervous system. Neural sensory receptors for blood pressure, named baroreceptors, are in the arch of the aorta and at the bifurcation of the common carotid artery.
Baroreceptor afferent neurons travel to the brain stem in cranial nerves IX and X of the parasympathetic system. Their destination is the brain stem nuclei that regulate sympathetic and parasympathetic output to the heart.
To balance dilation of skeletal muscle arteries, sympathetic neural activity causes vasoconstriction of blood vessels elsewhere as is illustrated below. As exercise proceeds sensory afferents from skeletal muscle and the baroreceptors modify the process of central command.
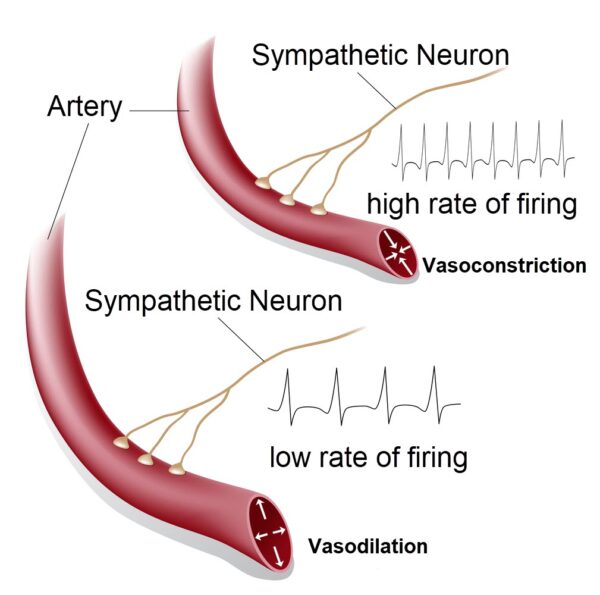
A high rate of sympathetic firing constricts the arteries, illustration by Alila Medical Media, Shutterstock.com
Exercise supplies one example of cardiovascular/nervous collaboration
Exercise physiology supplies one example of the dynamic interface between the cardiovascular system and the nervous system.
Cardiovascular responses to exercise are well documented. However, the concept of brain’s central command during exercise is still a work in progress. Because the central command process at the initiation of exercise depends on memory of previous experience, the intensity of the response to exercise varies by individual.
The role of the autonomic nervous system in control of heart rate, cardiac output, bronchial dilation, and blood pressure regulation is better understood than how memory anticipates the required cardiac output and lung ventilation.
However, there is always more to learn about exercise physiology. For example, recent data suggest exercise also activates the pleasure pathways of the brain reducing chronic stress. And you have probably heard the phrase “Addicted to exercise.”
Further Reading
Tips for How to Study the Cardiovascular System
Smooth Muscle Anatomy and Physiology
Do you have questions?
Send me an email with your questions at DrReece@MedicalScienceNavigator.com or put them in the comment box. I always read my mail and answer it. Please share this article with your fellow students taking anatomy and physiology by clicking your favorite social media button.
Margaret Thompson Reece PhD, physiologist, former Senior Scientist and Laboratory Director at academic medical centers in California, New York and Massachusetts is now Manager at Reece Biomedical Consulting LLC.
She taught physiology for over 30 years to undergraduate and graduate students, at two- and four-year colleges, in the classroom and in the research laboratory. Her books “Physiology: Custom-Designed Chemistry”, “Inside the Closed World of the Brain”, and her online course “30-Day Challenge: Craft Your Plan for Learning Physiology”, and “Busy Student’s Anatomy & Physiology Study Journal” are created for those planning a career in healthcare. More about her books is available at https://www.amazon.com/author/margaretreece. You may contact Dr. Reece at DrReece@MedicalScienceNavigator.com, or on LinkedIn.
Dr. Reece offers a free 30 minute “how-to-get-started” phone conference to students struggling with human anatomy and physiology. Schedule an appointment by mail at DrReece@MedicalScienceNavigator.com.


Comments
Exercise Physiology — No Comments
HTML tags allowed in your comment: <a href="" title=""> <abbr title=""> <acronym title=""> <b> <blockquote cite=""> <cite> <code> <del datetime=""> <em> <i> <q cite=""> <s> <strike> <strong>