Hormone Regulation of Plasma Calcium: Human
Hormone feedback control of blood calcium
For students new to endocrinology, hormone feedback control of plasma calcium by parathyroid hormone is a good place to start learning the endocrine system. Blood calcium regulation is simpler than other aspects of endocrinology, because parathyroid hormone regulation does not include a brain component.
It is critical that free calcium ion [Ca++] in blood plasma, and therefore in interstitial fluid around cells, is maintained at a steady level. Action potentials of cardiac muscle require a higher concentration of Ca++ in the extracellular fluid than within the cell. Likewise, release of neurotransmitter at neuron synapses depends upon a reliable diffusion of Ca++ into neuron terminals through voltage-gated calcium ion channels.
Ca++ moves freely through blood capillary endothelial membranes between blood and the interstitial fluid. Thus, the concentration of Ca++ remains similar in blood and interstitial fluid. Calcium enters the body regularly from the diet through the gastrointestinal tract. When dietary calcium drops, or if the kidney’s ability to reabsorb Ca++ after blood filtration becomes impaired, bone acts as a Ca++ reservoir. Crystals of bone’s calcium phosphate are broken down to maintain calcium ion’s plasma set point.
Parathyroid hormone
Blood Ca++ regulation begins at the parathyroid gland. The parathyroid gland, composed of four small structures, sits on the surface of the thyroid gland. The hormone it secretes is called parathyroid hormone.
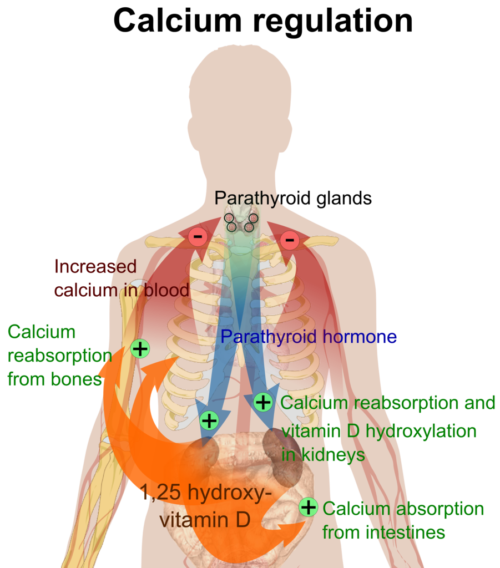
The rate of parathyroid hormone secretion increases above its constant basal rate when Ca++ in plasma falls below a critical level. Blood flow delivers parathyroid hormone to bone compartments. Parathyroid hormone receptors in bone exist on the surface of osteoblasts, the cells that build bone. Increased parathyroid hormone stimulates osteoblast secretion of secondary molecules to trigger osteoclasts to breakdown bone’s calcium phosphate crystals.
Plasma concentrations of Ca++ and phosphate ion rise in the presence of parathyroid hormone at bone. To prevent recrystallization of calcium phosphate, the phosphate ion must be eliminated. To accomplish this parathyroid hormone has an additional effect at the kidney. At the distal tubules and collecting duct of the nephrons parathyroid hormone inhibits reabsorption of phosphate ions back into blood.
Parathyroid hormone at the kidney also stimulates kidney conversion of the inactive form of vitamin D in blood to its active form. In turn, an increased amount of active vitamin D binds to its receptors in intestinal cells and enhances absorption of Ca++ from digested food.
Parathyroid hormone regulation
The cells of the parathyroid gland have a receptor on their surface for binding Ca++. This calcium-sensing receptor connects to intracellular pathways regulating the synthesis of parathyroid hormone. When interstitial fluid Ca++ rises above 10 mg/dl due to bone re-absorption and increased uptake from the intestine, calcium-sensing receptor activity slows parathyroid hormone synthesis and release. Parathyroid hormone falls to its low basal level in blood.
The adjacent thyroid gland also produces a hormone named calcitonin. Calcitonin works in opposition to parathyroid hormone to lower plasma Ca++ when it is too high. While calcitonin paired with parathyroid hormone remains an important regulator of plasma Ca++ in some animals, calcitonin does not appear to play a significant role in human Ca++ regulation. In those where calcitonin has a role, it inhibits osteoclast activity by binding to a receptor embedded in the osteoclast membrane. And, it inhibits re-absorption of Ca++ and phosphate ion.
Be sure to learn parathyroid hormone regulation of blood calcium before tackling the rest of endocrinology. Regulation of the body by other endocrine hormones includes the brain a part of the feedback loops, making the story more complicated.
More endocrine physiology:
Do you have questions?
Send me an email with your questions at DrReece@MedicalScienceNavigator.com, or put them in the comment box. I always read my mail and answer it. Please share this article with your fellow students taking anatomy and physiology by clicking your favorite social media button.
Margaret Thompson Reece PhD, physiologist, former Senior Scientist and Laboratory Director at academic medical centers in California, New York and Massachusetts is now Manager at Reece Biomedical Consulting LLC.
She taught physiology for over 30 years to undergraduate and graduate students, at two- and four-year colleges, in the classroom and in the research laboratory. Her books “Physiology: Custom-Designed Chemistry”, “Inside the Closed World of the Brain”, and her online course “30-Day Challenge: Craft Your Plan for Learning Physiology”, and “Busy Student’s Anatomy & Physiology Study Journal” are created for those planning a career in healthcare. More about her books is available at https://www.amazon.com/author/margaretreece. You may contact Dr. Reece at DrReece@MedicalScienceNavigator.com, or on LinkedIn.
Dr. Reece offers a free 30 minute “how-to-get-started” phone conference to students struggling with human anatomy and physiology. Schedule an appointment by email at DrReece@MedicalScienceNavigator.com.


Comments
Hormone Regulation of Plasma Calcium: Human — No Comments
HTML tags allowed in your comment: <a href="" title=""> <abbr title=""> <acronym title=""> <b> <blockquote cite=""> <cite> <code> <del datetime=""> <em> <i> <q cite=""> <s> <strike> <strong>