How to study gastrointestinal physiology
In a previous article, Human Digestion: Main & Accessory Organs I discussed the exocrine secretions of the gastrointestinal system and how the cardiovascular system supports exocrine activity. In this article, Gastrointestinal Hormones for Digestion & Fasting, I will review the digestive tract use of the hormone secretions by its endocrine glands.
This is the third in a series of articles about the gastrointestinal system. The two previous articles in this series, Gastrointestinal Tract Neural Regulation and Human Digestion: Main & Accessory Organs may be found by clicking on the titles.
I strongly encourage you to approach your study of the physiology of each anatomic system by first asking how the nervous system supports its purpose. Then research the contribution of the cardiovascular system. And, finally sort out how each system is regulated by endocrine hormones.
Gastrointestinal hormones
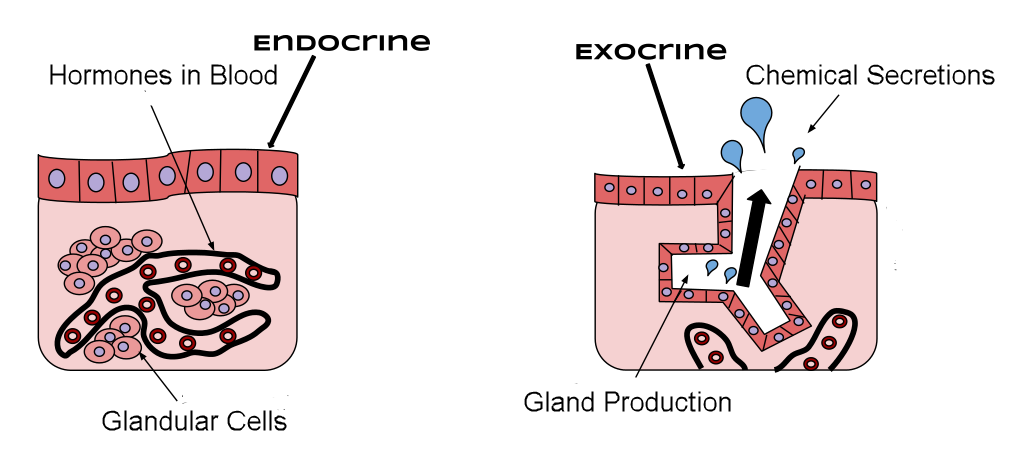
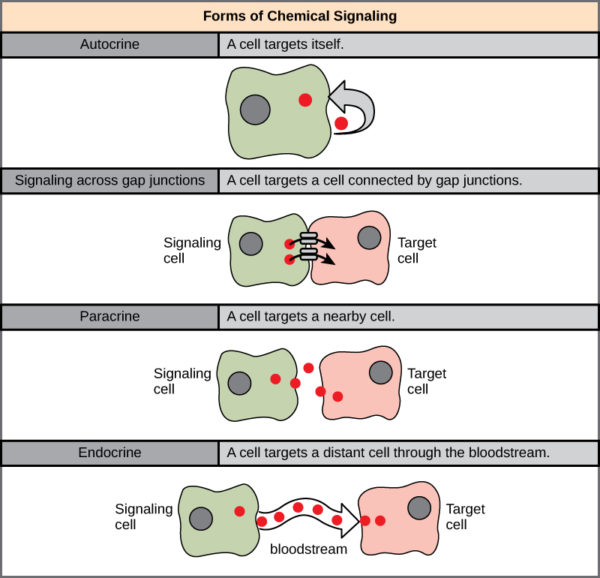
Endocrine hormones are classically defined to be chemicals that are secreted into the blood stream for delivery to their target tissue. This discussion of gastrointestinal hormones will be limited to the digestive tract endocrine hormones.
You may read elsewhere about more gastrointestinal tract ‘hormones’ that participate in digestion that are not secreted into blood for delivery to their target. Those hormones do not match the classical definition of ‘endocrine hormone’. Rather they act as paracrine and autocrine hormones. At present count there are about 30 paracrine and autocrine chemicals that locally regulate digestion.
More about how the endocrine system is organized to include endocrine hormones, paracrine hormones and autocrine hormones may be found in an earlier article, Endocrine System Overview by clicking the title.
The digestive system has six endocrine hormones that fit the classical definition of hormones secreted into the blood. They are gastrin, cholecystokinin (CCK), secretin, glucose-dependent insulinotropic peptide (GIP), motilin and ghrelin. Gastrin, CCK and GIP are hormones of feasting. Motilin and ghrelin are hormones of fasting.
Enteroendocrine cells
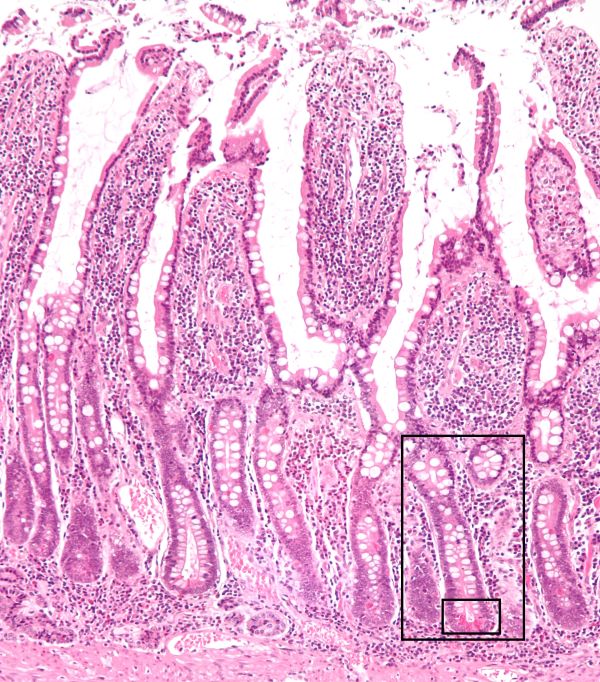
Specialized columnar epithelial cells of the GI tract mucosa, enteroendocrine cells, synthesize the tract’s hormones. Enteroendocrine cells originate from the pluripotent stem cells located at the base of the crypts between intestinal villi.
The entire epithelium of the intestinal villi renews every 4-5 days with new cells moving up from the crypts at the bottom. The dying cells are sloughed off into the lumen of the tract. As new cells move from the bottom toward the lumen, they mature into absorptive or secretory types.
Enteroendocrine cells are located along the bottom half of the villi. They are generally isolated from each other among other secretory and absorptive cells. They are in greater density in the mucosa at the proximal end of the tract, the stomach, than at the distal end, the colon.
The various types of enteroendocrine cells are identified and named for the type of secretory granules they contain. Immunohistochemical staining distinguishes one kind of hormone secretory granule from another.
Digestive hormones
Gastrin
Gastrin is a peptide hormone. Peptides are a relatively short string of amino acids. Gastrin is produced by the G-Cells of the gastric pits at the pyloric end of the stomach and in the first section of the small intestine, the duodenum. Gastrin release into blood is stimulated by ingestion of protein, gastric distension, and an elevated intestinal pH.
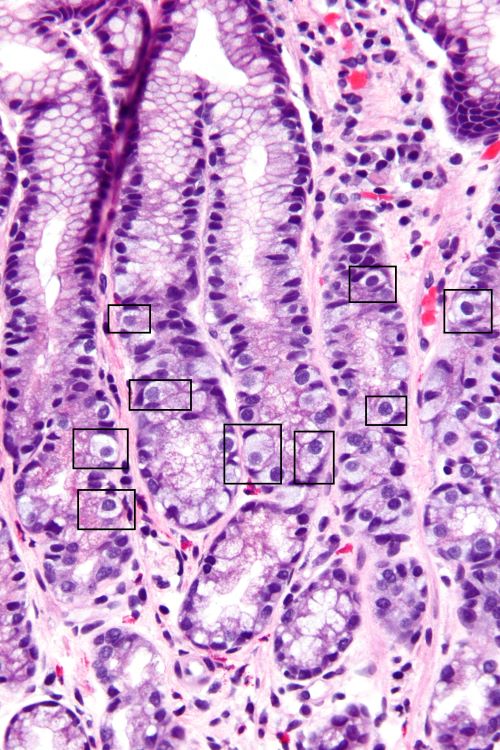
Photomicrograph of the gastric antrum showing abundant fried egg-lik G-Cells outlined by black boxes, Nephron/Wikimedia Commons
Gastrin has several functions. It enhances gastric mucosal cell proliferation, gastric motility and secretion of hydrochloric acid into the stomach. At the parietal cell membrane, gastrin increases the K+/H+ ATPase pumps supplying hydrogen ions to the stomach. At the pancreas, Gastrin binds to acinar cells that synthesize and secrete pancreatic digestive enzymes inducing their secretion.
Secretin
In 1905 studies of how the pancreas secreted digestive juices in response to food entering the duodenum lead British physiologists, William Bayliss and Ernest Starling, to coin the term hormone for a molecule they named secretin.
Like gastrin, secretin is a peptide hormone. It is produced by the S-Cells of the intestinal mucosa of the duodenum and jejunum. It is secreted into blood in response to low duodenum pH in the range of 2 – 4.5. When pH in the duodenum rises above 4.5, secretin release ceases.
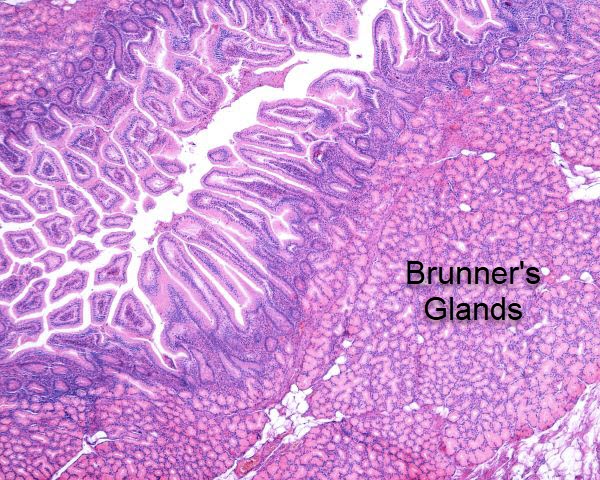
In the digestive process, secretin hormone regulates cells of the stomach, pancreas, liver and Brunner’s glands of the duodenum submucosa. Brunner’s glands secrete an alkaline mucus that coats and protects the duodenum’s epithelial cells from acid in the chyme delivered by the stomach through the pyloric valve.
Secretin reduces acid secretion by the parietal cells of the stomach. It accomplishes this by inhibiting gastrin secretion of the G-Cells and by directly affecting the cellular pathways of the parietal cells.
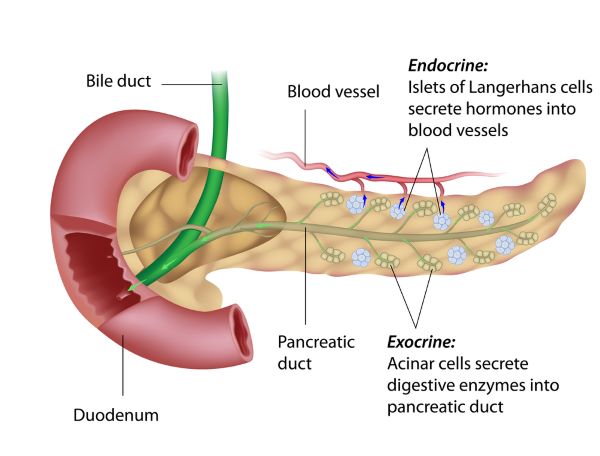
Secretin also targets the acinar cells of the pancreas to stimulate their secretion of a bicarbonate-rich watery solution that flows to the intestine through the pancreatic duct. Bicarbonate establishes a pH favorable for enzymatic breakdown of food particles.
Secretin likewise stimulates bile duct cells to secrete water and bicarbonate. This expands the volume of the bile and increases its flow to the small intestine through the bile duct. Bile is required for emulsification of fat so that lipase may act efficiently in breaking down fat molecules.
Cholecystokinin (CCK)
Cholecystokinin, also called pancreozymin, is a peptide hormone of the gastrointestinal tract that stimulates digestion of fat and protein. It is synthesized and secreted by the I-Cells of the duodenum and jejunum. CCK is released into blood in response to the presence of fatty acids and certain peptides found in the chyme delivered by the stomach to the duodenum.
At the pancreas, cholecystokinin stimulates the acinar cells to release a fluid rich in digestive enzymes that catalyze the digestion of fat, protein and carbohydrate. As the levels of undigested fat, protein and carbohydrate drop in the small intestine the release of CCK is turned off. Trypsin, a protease released by the pancreatic acinar cells hydrolyzes the peptides signaling release of CCK.
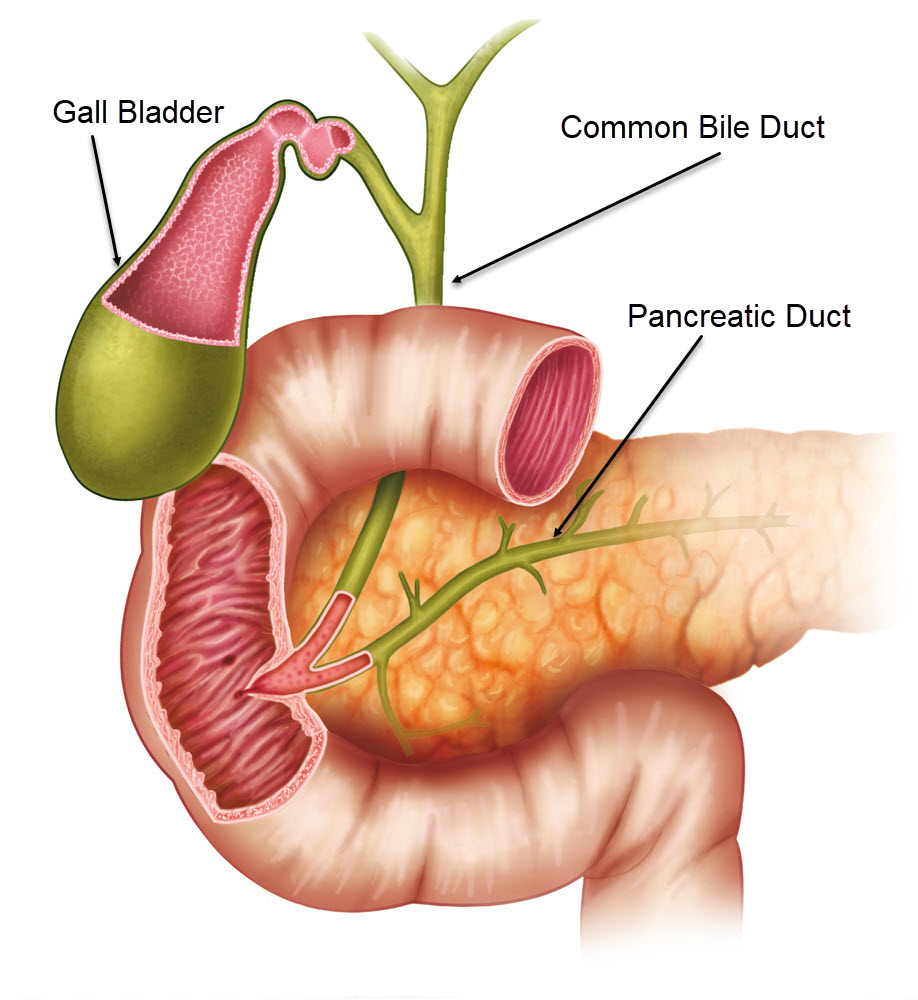
Common bile duct of liver joins pancreatic duct as they enter duodenum, ilusmedical/Shutterstock.com
At the liver, CCK causes increased production of bile and promotes contraction of the gall bladder and the common bile duct. It relaxes the sphincter of Oddi allowing bile to flow into the duodenum. As bile flows through the bile ducts, it accumulates a secretin-induced watery secretion from bile duct epithelial cells. Secretin augments the CCK-induced contraction of the gall bladder.
Glucose-dependent insulinotropic peptide (GIP)
The main role of glucose-dependent insulinotropic peptide hormone (GIP) is to stimulate insulin secretion at the pancreas. It is synthesized and released by the enteroendocrine K-Cells of the duodenum and jejunum. GIP release to blood is stimulated by a large amount of glucose in the duodenum.
GIP binds to membrane receptors of the pancreas beta cells and induces them to secrete insulin.
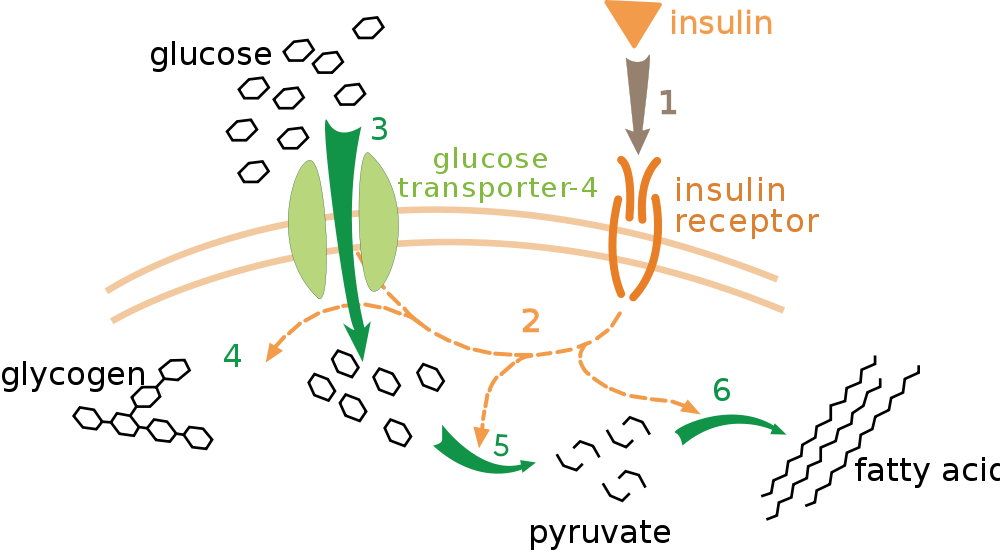
Effect of insulin on glucose uptake and metabolism by liver, fat and skeletal muscles, Public Domain/Wikimedia Commons
Insulin promotes the absorption of glucose from blood by the liver, fat and skeletal muscles. In liver and muscle, glucose is converted into the storage form glycogen. In fat it is stored as triglyceride.
Fasting hormones
Motilin
Motilin, a 22 amino acid peptide is a fasting hormone. It is produced by the Mo-Cells of the duodenum and jejunum. It is secreted into blood during the period between the times when there is active digestion of food in the gastrointestinal tract. The identity of the exact molecular stimulus for motilin secretion is not yet known.
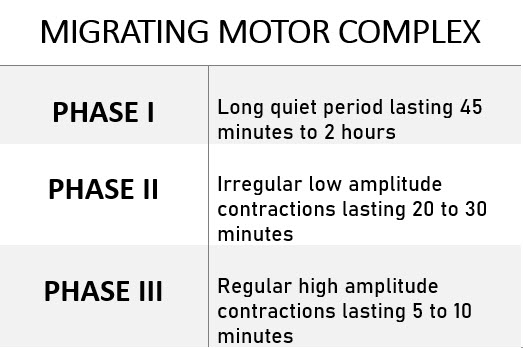
Motilin’s main function is to increase the strength of the migrating motor complex pattern of gut motility during the fasting period. The migrating motor complex is an orderly set of contractions of gastrointestinal muscles that clears undigested material from the tract. For more about how the enteric nervous system controls contraction of the gut, please read Gastrointestinal Tract Neural Regulation.
The full sequence of the migrating motor complex occurs in three phases that takes about 1.5 – 3.0 hours. It begins in the stomach and ends at the terminal ilium where it pushes material through the ileocecal sphincter into the colon. Motilin is thought to be the primary regulator of the Phase III activity.
Ghrelin
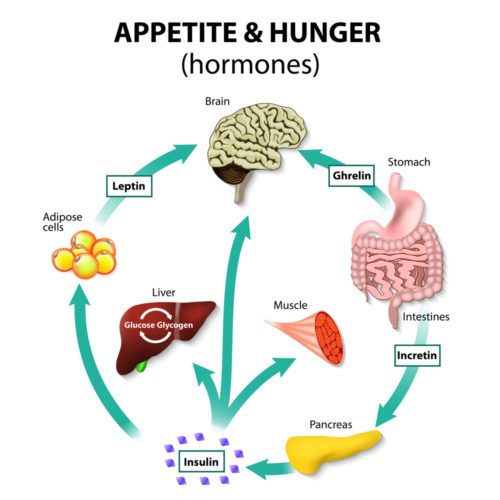
In the gastrointestinal tract, ghrelin is synthesized and secreted by the X/A-like-Cells of the stomach. It is a 28 amino acid peptide that is highest in blood before a meal when a person is hungry and lowest after eating. It has been called the hunger hormone even though it is produced by a variety of organs and has many functions outside fasting.
During fasting, ghrelin actives cells in the hypothalamus and other areas of the brain. It is the neurons of the hypothalamic arcuate nucleus that are responsible for appetite. In addition to increasing appetite, ghrelin stimulates brain pathways involved in reward behavior.
When it comes to hunger and appetite, ghrelin is not the sole influence on the brain’s response. The pathways illustrated here will only become more complex soon as scientists continue their study of the brain’s regulation of the gastrointestinal system.
Digestive system & central nervous system
The three articles in this series introduce you to the basic physiology of the digestive system. Dividing the digestive system into neural, cardiovascular/exocrine and endocrine sections for study simplifies learning the complex organization of this multi-organ system.
But before leaving this topic, I want to emphasize the close working relationship that exists between the digestive system and the central nervous system. The enteric nervous system develops in the embryo in parallel with the central nervous system. Hunger and appetite are constructs of the conscious brain that are influenced many sensory pathways as well as by the above describes enteroendocrine hormones.
Some of the paracrine factors that influence health of gastrointestinal tract are found in the brain functioning as neurotransmitters. While management of moving food through the GI tract is primarily accomplished by the enteric nervous system, the central nervous system constantly monitors its affairs through multiple sensory pathways. The brain can override the enteric nervous system when infectious particles and tainted food enter the digestive system with the vomiting reflex.
Further reading
Gastrointestinal Tract Neural Regulation
Human Digestion: Main & Accessory Organs
Do you have questions?
Send me an email with your questions at DrReece@MedicalScienceNavigator.com or put them in the comment box. I always read my mail and answer it. Please share this article with your fellow students taking anatomy and physiology by clicking your favorite social media button.
Margaret Thompson Reece PhD, physiologist, former Senior Scientist and Laboratory Director at academic medical centers in California, New York and Massachusetts is now Manager at Reece Biomedical Consulting LLC.
She taught physiology for over 30 years to undergraduate and graduate students, at two- and four-year colleges, in the classroom and in the research laboratory. Her books “Physiology: Custom-Designed Chemistry”, “Inside the Closed World of the Brain”, and her online course “30-Day Challenge: Craft Your Plan for Learning Physiology”, and “Busy Student’s Anatomy & Physiology Study Journal” are created for those planning a career in healthcare. More about her books is available at https://www.amazon.com/author/margaretreece. You may contact Dr. Reece at DrReece@MedicalScienceNavigator.com, or on LinkedIn.
Dr. Reece offers a free 30 minute “how-to-get-started” phone conference to students struggling with human anatomy and physiology. Schedule an appointment by email at DrReece@MedicalScienceNavigator.com.