Endocrine regulation of body function
In A&P courses, the endocrine system is usually taught late in the second semester, because of its many parts, complex regulation, and the increasing number of molecules that fit under the definition of an endocrine hormone.
This article organizes the basic information you need to further explore the physiology of this amazing human body system.
Endocrine regulation of physiology adheres to a slower time course than that of the neural and cardiovascular systems. The nervous system operates in milliseconds, and the cardiovascular system uses moment-to-moment management. Except in some emergencies, endocrine regulation occurs over hours, days, months and occasionally years.
However, the large role played by the brain in long-term endocrine regulation, discovered late in the 20th century, blurs the distinction between the nervous system and the endocrine system.
Endocrine system components
The three basic components of the endocrine system are molecules that fit the definition of hormone, hormone secreting cells named endocrine glands, and distant hormone responding cells called target cells.
Hormones
A hormone is defined to be a molecule secreted into the blood stream that is active at a distant site in the body. The endocrine system depends upon the cardiovascular system to carry its hormones to distant target cells.
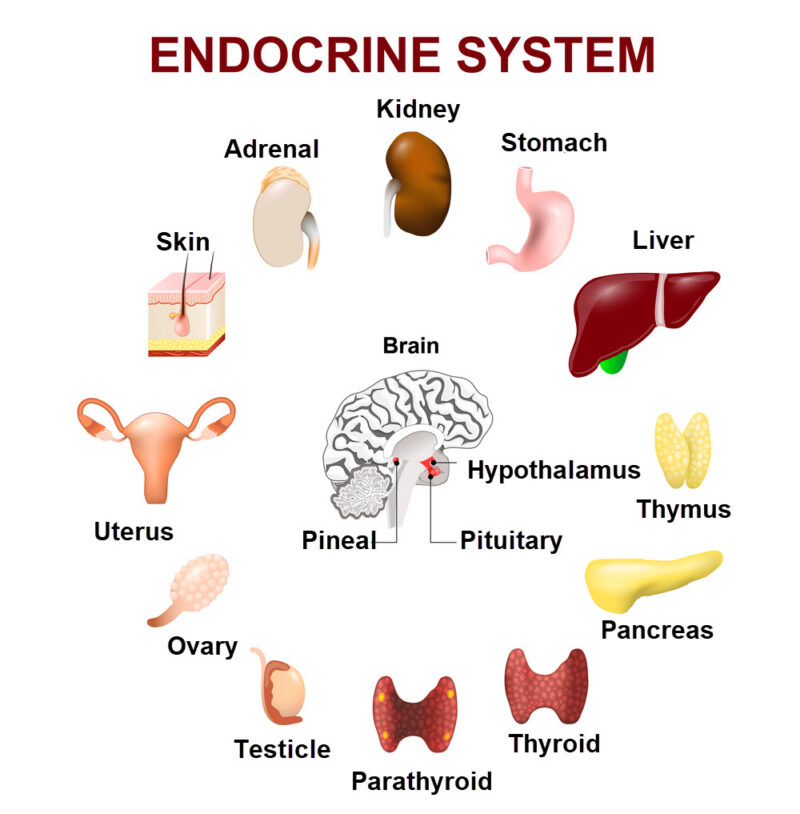
Many different cell types secrete hormones into blood. Organs participating in the endocrine system are illustrated in the image below.
Endocrine glands
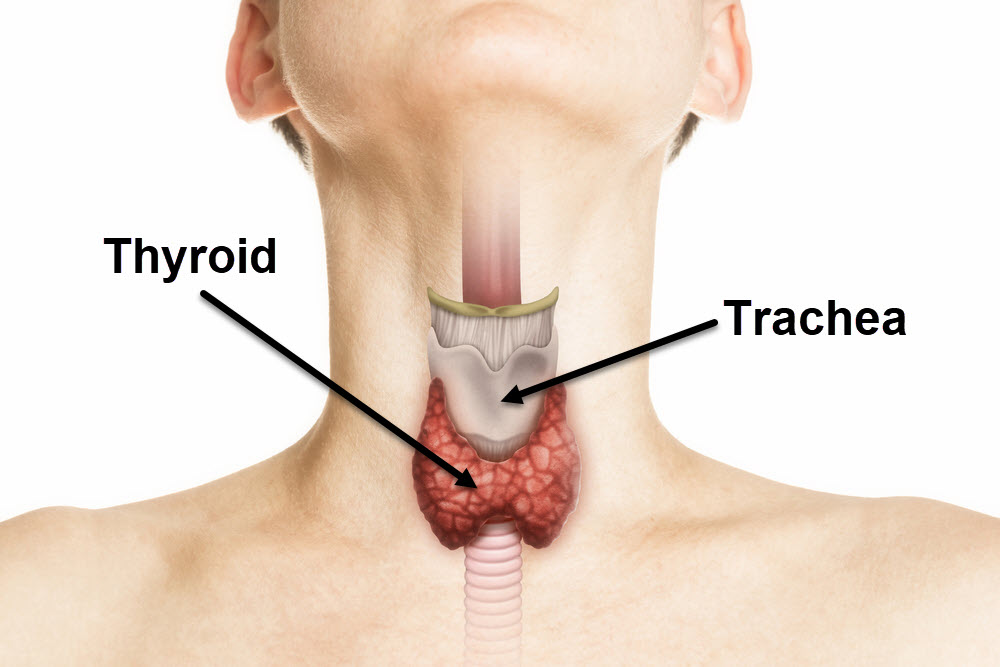
Some endocrine glands are clustered into distinct structures, separate from the surrounding tissue. These easily identified clusters of hormone secreting cells are traditional endocrine organs, like the thyroid gland illustrated below.
Traditional endocrine glands are scattered throughout the human body. These endocrine organs provided the earliest understanding of how the endocrine system functioned. In addition to the thyroid gland this group includes the parathyroid gland, the pineal gland, the pituitary gland, the adrenal gland, the pancreas, the thymus, the ovaries, and the testes.
Non-traditional endocrine glands may be single cells or small clusters of cells embedded in large organs. An example is secretion of the hormone gastrin by the stomach and by the first section of the small intestine, the duodenum.
Gastrin hormone is synthesized and secreted by small cells named G-cells. G-cells of the stomach are found in the gastric pits. In the photomicrograph of stomach tissue below, the gastrin secreting cells are outlined by black boxes.
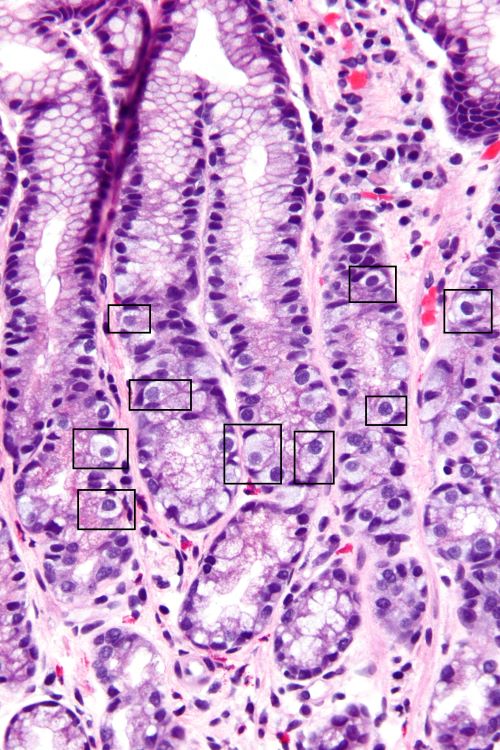
Photomicrograph of the gastric antrum showing abundant fried egg-lik G-Cells outlined by black boxes, Nephron/Wikimedia Commons
Gastrin release into blood capillaries is stimulated by ingestion of protein, by gastric distension, and by an elevated intestinal pH. Gastrin is carried by blood to the pancreas. In response, the acinar cells of the pancreas synthesize and secrete digestive enzymes for delivery to the small intestine.
Hormone target cells
A hormone’s target cell is defined to be a cell that can respond to the hormone’s presence in blood. The acinar cells of the pancreas are target cells for gastrin.
Target cells respond to hormones because they contain proteins that recognize the shape of the hormone molecule. Cell proteins that recognize hormones are called hormone receptors.
The name hormone originates from a Greek word that means to ‘set in motion’. If a cell has a receptor for the presence of a particular hormone, then that hormone is capable of setting in motion the cell’s molecular pathways to create a specific effect.
Endocrine brain and the pituitary gland
The brain is a central component of the nervous system. Thus, the discovery that some brain neurons are also part of the endocrine system was a surprise. Naming the molecules released by brain neuron terminals into blood capillaries as hormones was resisted for some time.
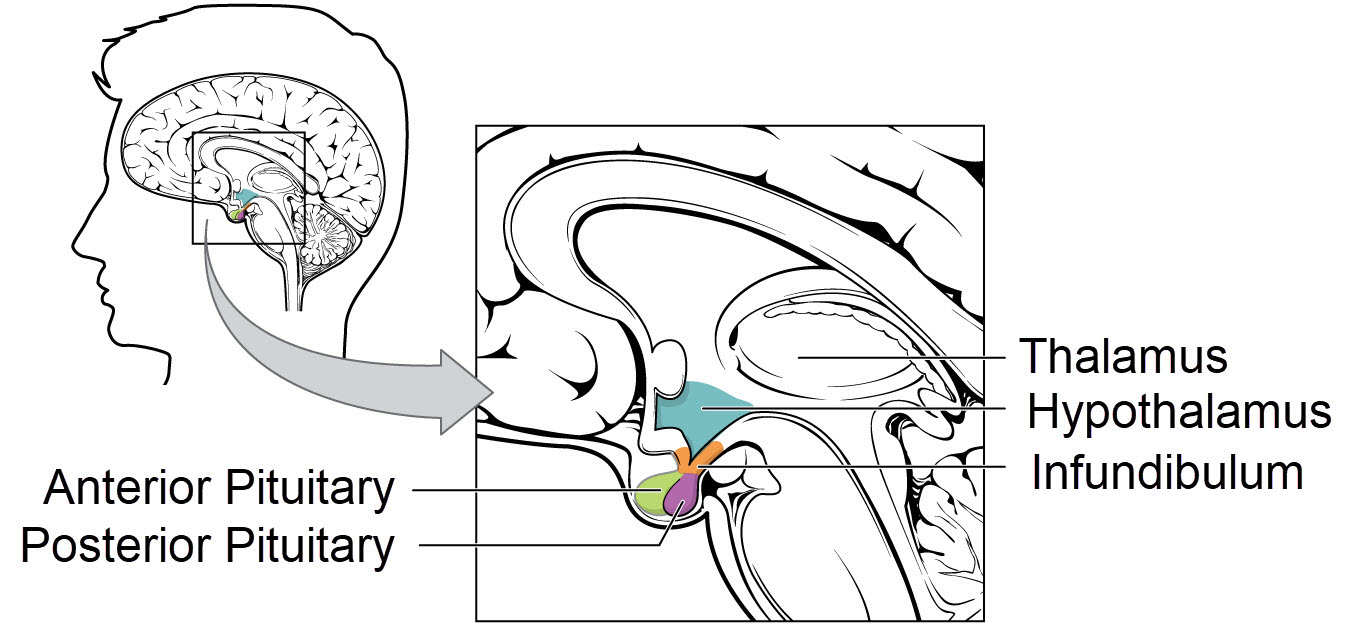
This unexpected neural/endocrine arrangement opened a new division of endocrinology named neuroendocrinology. Brain’s neuroendocrine structures are the hypothalamus and the posterior part of the pituitary gland.
The anatomy of the endocrine brain and pituitary gland is illustrated below.
Hypothalamus
The hypothalamus of the brain is a group of deep brain neuron cell clusters, called brain nuclei. A portion of hypothalamic neurons regulate synthesis and release of anterior pituitary gland hormones.
The hypothalamic neurons release small peptides from their terminal ends into the capillaries of the infundibulum. The infundibulum is a stalk of tissue connecting the hypothalamus and anterior pituitary gland. The infundibular capillaries connect with the pituitary’s capillary bed.
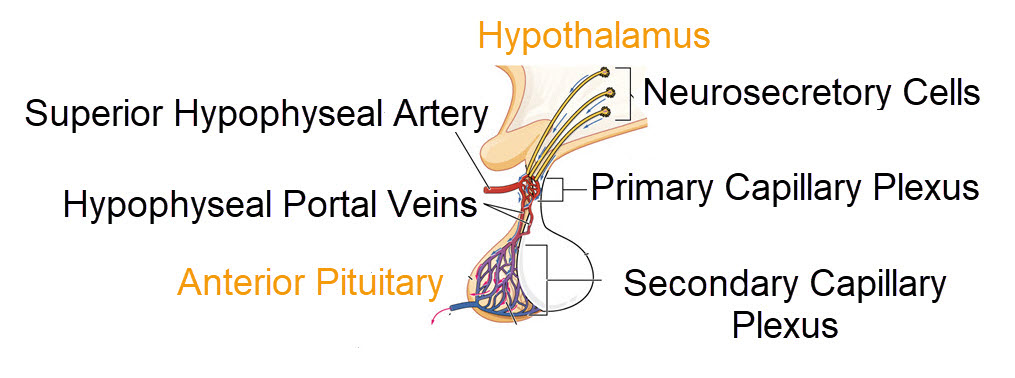
Infundibular vessels that deliver hypothalamic releasing hormones to the anterior pituitary capillaries, Open Stax College, Wike Media Commons
Hypothalamic peptides regulating the anterior pituitary are called releasing hormones, because they increase the synthesis and release of anterior pituitary hormones. Secretion of hypothalamic releasing hormones occurs in response to a wide array of sensory information arriving at the brain from multiple body regions.
Anterior pituitary gland
The pituitary gland has three lobes based upon its histology, anterior/pars distalis, posterior/pars nervosa, and intermediate/pars intermedia. The anterior lobe secretes 6 different protein hormones into the blood capillaries perfusing it.
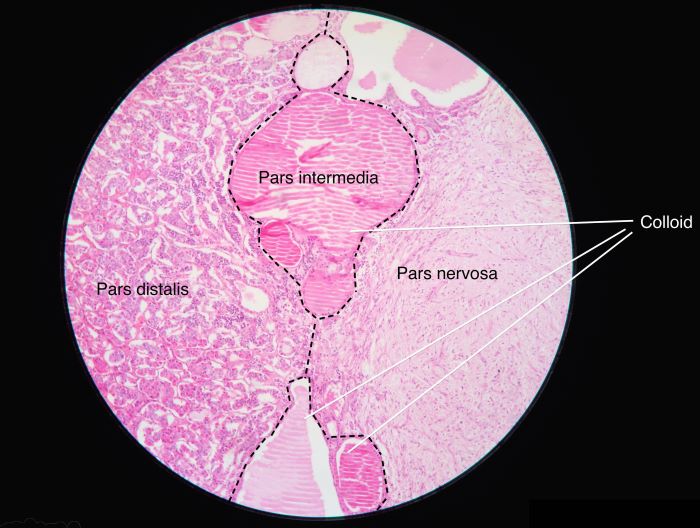
The pars distalis is also commonly called the anterior pituitary. The pars nervosa is the posterior pituitary, Athikhun.suw, Wikimedia Commons
Anterior pituitary gland hormones are carried by the vasculature to other hormone producing glands, which are distributed throughout the body. Anterior pituitary gland hormones are said to be trophic to the glands they target, because they set in motion hormone synthesis and secretion pathways in the targeted glands.
Posterior pituitary gland
The posterior pituitary gland is composed of the terminal ends of brain neurons whose cell bodies lie in the hypothalamus. Posterior pituitary gland neurons originate in a different hypothalamic nucleus than those that secrete releasing hormones into the infundibular capillaries.
The two posterior pituitary hormones, oxytocin and vasopressin, are released directly into the systemic vasculature. The targets of oxytocin are the reproductive organs, the uterus at parturition and the breast during lactation. A major target of vasopressin is the kidney.
Intermediate pituitary gland
The intermediate pituitary gland secretes a hormone named melanocyte stimulating hormone. In humans, this gland contains a collection of colloid structures forming a boundary between the anterior and posterior pituitary glands.
The intermediate pituitary gland in adult humans is small, and it is not thought to secrete hormone. However, the intermediate pituitary gland plays an important role in the endocrine system of other species.
Hormone classes
Hormones’ ever-expanding population
Separating hormones into classes is difficult because of the ever-expanding population of ‘new’ hormones.
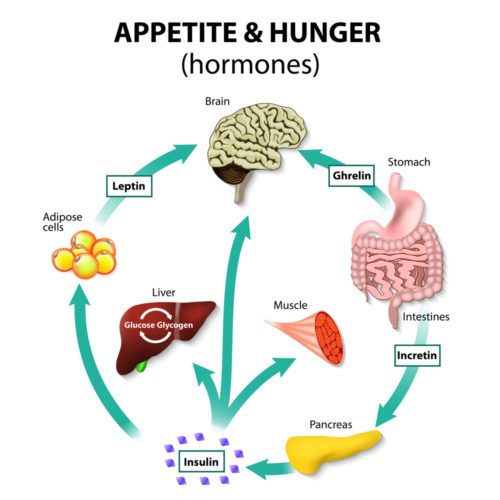
The expanding population of endocrine hormones includes among others those controlling appetite and hunger, the heart’s atrial natriuretic peptide, and bone’s osteocyte secretion of the hormone FGF23.
With the ever-expanding population of hormones, it is simplest now to divide hormones into two classes; 1) those that bind to hormone receptor proteins embedded in a cell’s plasma membrane, and 2) those that penetrate the cell plasma membrane to bind to intracellular hormone receptor proteins.
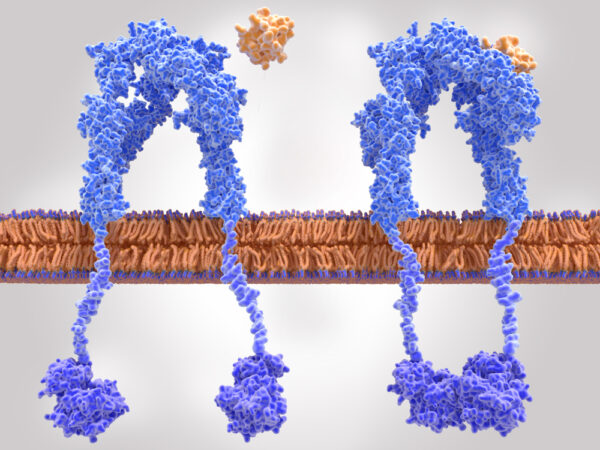
Plasma membrane hormone receptors
Plasma membrane hormone receptors bind small hydrophilic hormone molecules, amino-acid-derivative hormones, peptide hormones, and protein hormones. Hormones using plasma membrane hormone receptors remain outside the cells they target. Below is an illustration of the insulin receptor protein embedded in a cell’s plasma membrane.
Notice that this is a two-part receptor, and that the intracellular portions are distant from each other. When insulin, the yellow ball, binds to one part of the receptor, the intracellular tails of the two parts move together.
The interaction of the two intracellular tails of the insulin receptor sets in motion particular intracellular pathways. In this case, the intracellular activity moves glucose transporters into the plasma membrane, enhancing the cell’s uptake of glucose.
Intracellular hormone receptors
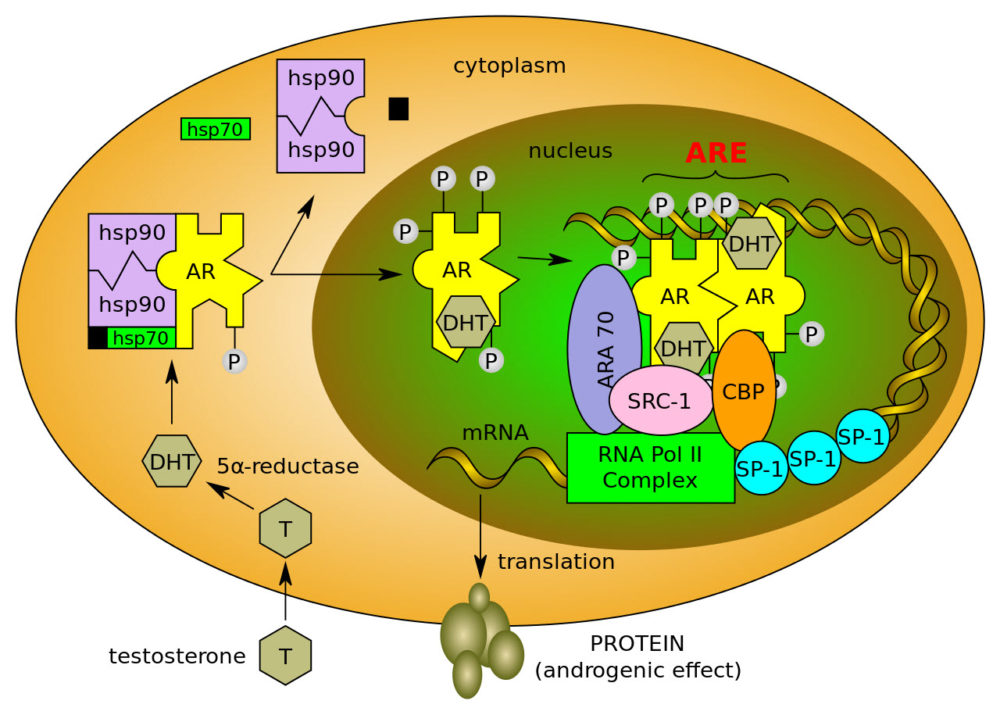
Hormones that are derivatives of cholesterol enter cells and bind to intracellular hormone receptors. Cholesterol-derivative hormones are called steroid hormones. Steroid hormones are synthesized in the adrenal glands, the ovaries, the testes, and the brain.
A testicular cell’s response to the entry of testosterone is illustrated below. In this cell, testosterone regulates the expression of more than 150 different genes and their product proteins.
Thyroid hormone is an exception to a general rule that amino-acid-derivative hormones bind to plasma membrane hormone receptors. As illustrated below thyroid hormone (T3) uses a transporter protein to enter its target cell. It is also unusual that, after entry, thyroid hormone activates both the cell’s cytoplasmic and genomic pathways.
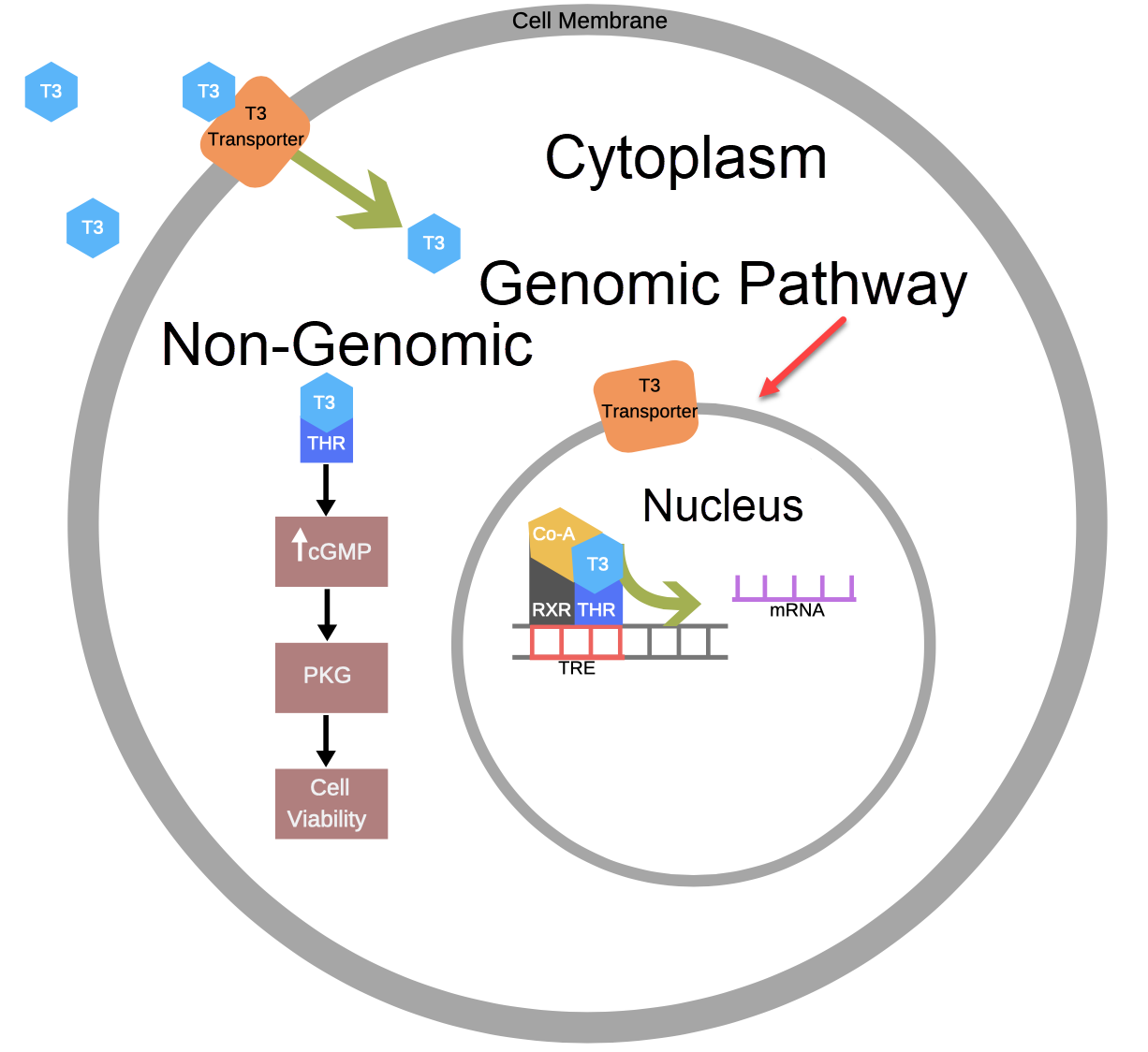
Thyroid hormone activates both genomic and non-genomic intracellular pathways, Marianne D Sadar, Wiki Media Commons
Hormone feedback loop regulation
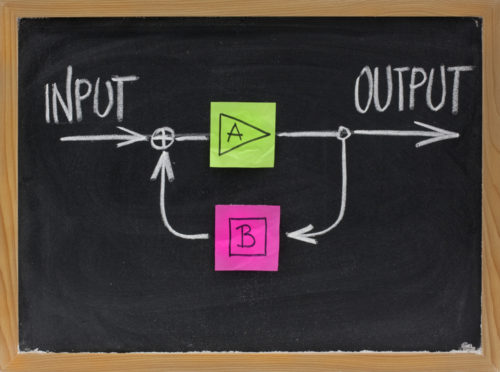
Hormone feedback regulation can be a difficult concept to understand at first, because many hormone feedback loops include multiple components. Fairly complex hormone feedback loops manage the endocrine hormones of the hypothalamus, pituitary, and their peripheral target organs.
However, there are endocrine hormone feedback loops that do not include the hypothalamus and pituitary. For example, feedback regulation of plasma calcium ion is managed by the parathyroid gland, bone, the intestine, and the kidney.
But the concept of feedback regulation is simple. As illustrated below, feedback loops include a portion of the output [B] of a process [A] returning to the input part of the system. Information carried by [B] modifies the input, increasing or slowing process [A], thus changing output [B].
In physiology, there is a predominance of negative feedback loop regulation. That is a portion of [B] signals either that the input is too high, and the process should be slowed, or that the process is not producing enough [B] and input should increase the process.
Positive feedback loops are rare in physiology because they cause things to break. Output [B] of a positive feedback loop urges the input to increase the rate of process [A] to ever higher levels of output. Positive feedback loops in human physiology include those that regulate contraction of the uterus during childbirth leading to expulsion of the infant, blood clotting, and monthly rupture of ovarian follicles releasing an ovum.
As you study the physiology of each anatomic system remember to look for the role of endocrine regulation there. Every cell in the body is affected by at least one or more hormones.
In summary
Endocrine regulation of body function includes molecules named hormones, secreted by endocrine glands into the blood, that cause an effect at their target cells. There is a large population of hormones synthesized and secreted by endocrine glands. Endocrine glands may be either single cells in larger organs, or distinct glandular structures scattered through the body, or brain hypothalamic neurons.
The population of hormones may be divided into two classes; 1) those that bind to hormone receptor proteins embedded in cell plasma membrane, and 2) those that penetrate the cell plasma membrane to bind to intracellular receptor proteins.
Negative hormone feedback loop regulation in physiology is common. Positive hormone feedback loop regulation is rare but used for reproductive processes and blood clotting.
More about endocrine hormones:
Hormone Regulation of Plasma Calcium: Human
Thyroid Hormone: What Does It Do?
Do you have questions?
Send me an email with your questions at DrReece@MedicalScienceNavigator.com or put them in the comment box. I always read my mail and answer it. Please share this article with your fellow students taking anatomy and physiology by clicking your favorite social media button.
Margaret Thompson Reece PhD, physiologist, former Senior Scientist and Laboratory Director at academic medical centers in California, New York and Massachusetts is now Manager at Reece Biomedical Consulting LLC.
She taught physiology for over 30 years to undergraduate and graduate students, at two- and four-year colleges, in the classroom and in the research laboratory. Her books “Physiology: Custom-Designed Chemistry”, “Inside the Closed World of the Brain”, and her online course “30-Day Challenge: Craft Your Plan for Learning Physiology”, and “Busy Student’s Anatomy & Physiology Study Journal” are created for those planning a career in healthcare. More about her books is available at https://www.amazon.com/author/margaretreece. You may contact Dr. Reece at DrReece@MedicalScienceNavigator.com, or on LinkedIn.
Dr. Reece offers a free 30 minute “how-to-get-started” phone conference to students struggling with human anatomy and physiology. Schedule an appointment by email at DrReece@MedicalScienceNavigator.com.