Thyroid Hormone: What Does It Do?
Thyroid hormone effects every cell
Thyroid hormone affects virtually every cell in the body. The thyroid system provides an example of how the endocrine system and the nervous system can functionally merge to achieve an objective. Thyroid hormone is crucial to growth, nutrient metabolism and body heat generation. Among numerous other things, it supports neuron maturation in infants and assists pituitary growth hormone in regulation of long bone growth.
Thyroid histology
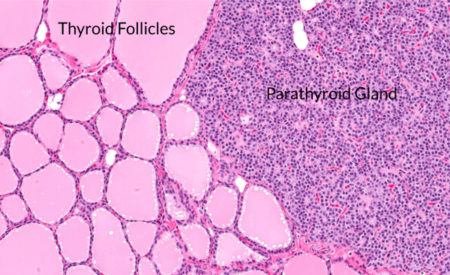
The thyroid gland, a butterfly-shaped organ situated on the anterior side of the neck, lies around the larynx and trachea below the Adam’s apple. On it lays the parathyroid gland.
At the microscopic level, the thyroid gland contains spherical structures called follicles where hormone is synthesized.
This photomicrograph shows a section of thyroid gland on the left and adjacent parathyroid gland on the right. Notice the structural difference in the two types of tissue. The center of each thyroid follicle is filled with a colloid material. In this section the thyroid cells are at the edges of the colloid.
Thyroid hormone synthesis
Follicle cells increase their synthesis of thyroid hormone in response to the blood presence of another hormone name Thyroid Stimulating Hormone (TSH). TSH is secreted by the pituitary gland and binds to a plasma membrane receptor on thyroid follicle cells. This sets in motion cellular pathways for the synthesis of thyroid hormone.
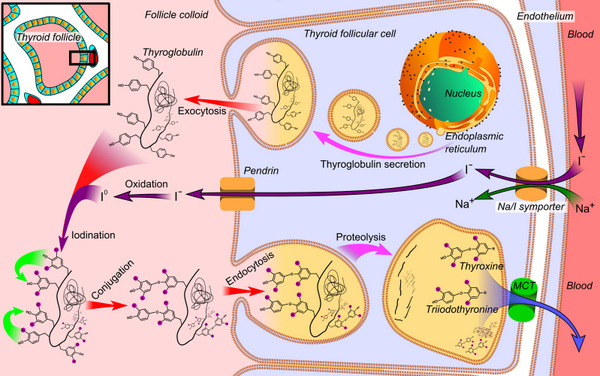
Steps in the synthesis of thyroid hormone and its release into blood, Public Domain/Wikimedia Commons
The initial step in thyroid hormone synthesis is production of a protein called thyroglobulin on the rough endoplasmic reticulum of the follicle cells. Thyroglobulin is transferred from the cell into the central colloid material by exocytosis. In the colloid of the follicle iodine is added to the thyroglobulin.
Iodide (I–) is pumped into the follicle cells from the capillaries supplying the follicle cells. As the concentration of I– increases in the cell it is passively transported into the central colloid. I– in the colloid is oxidized by an enzyme reaction to iodine (I0), a highly reactive molecule.
I0 combines with the many tyrosine residues of thyroglobulin. Iodinated thyroglobulin then reenters the follicle cell by endocytosis. Various cell enzymes that break apart proteins named proteases excise thyroxine (T4) with four attached iodine and triiodothyronine (T3) with three attached iodine. Cell membrane transporters then move T4 and T3 into blood capillaries.
Most, 80% of thyroid hormone leaving the gland is T4. In the blood, these small molecules are bound to large globular plasma proteins. Only about 1% of it is free and available for cellular uptake.
Thyroid hormone receptor
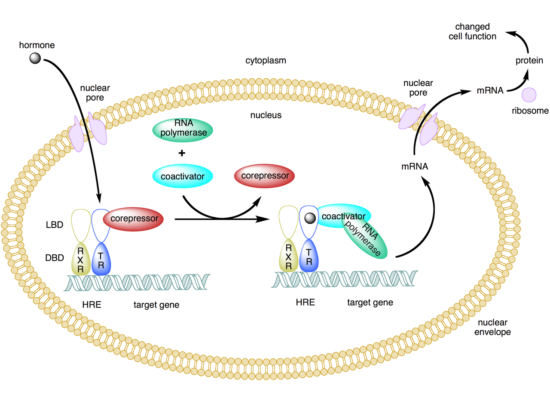
For a target cell to respond to a hormone it must have a receptor, a cell protein that binds to the hormone. Thyroid hormone receptors reside in the cell nucleus. Because thyroid hormone is not lipid soluble, it enters the target cell with the help of membrane transporters located in the plasma membrane to reach its receptors.
There are multiple types of thyroid hormone receptors. The number and type of thyroid receptor available varies by tissue. Two separate genes encode thyroid hormone receptors, TRHA and TRHB. TRHA produces six isoforms. All but 1, TRα1, lack a T3-binding domain and a DNA binding domain. The purpose of the short protein isoforms in thyroid hormone function is unclear. The THAB gene encodes fully functional receptors TRβ1 and TRβ2.
Thyroid hormone receptor may bind to DNA as a monomer (one thyroid receptor), a homodimer (two thyroid receptors bound together) or a hetero-dimer (one thyroid receptor plus a retinoid X receptor). The heterodimer with the retinoid X receptor is the major functional form of the thyroid hormone receptor.
The active form of thyroid hormone at nuclear receptors is T3. Iodine must be removed from T4 converting it to T3 for receptor binding to occur. There are 3 forms of the de-iodination enzymes within thyroid hormone target cells. These enzymes, depending upon their location and activity, allow thyroid hormone function to be regulated deferentially throughout the body.
Thyroid hormone regulation at the cellular level may take place at plasma membrane uptake, at enzymatic removal of iodine from T4 and T3, and in the nucleus depending upon the type of receptor available.
Thyroid hormone negative feedback
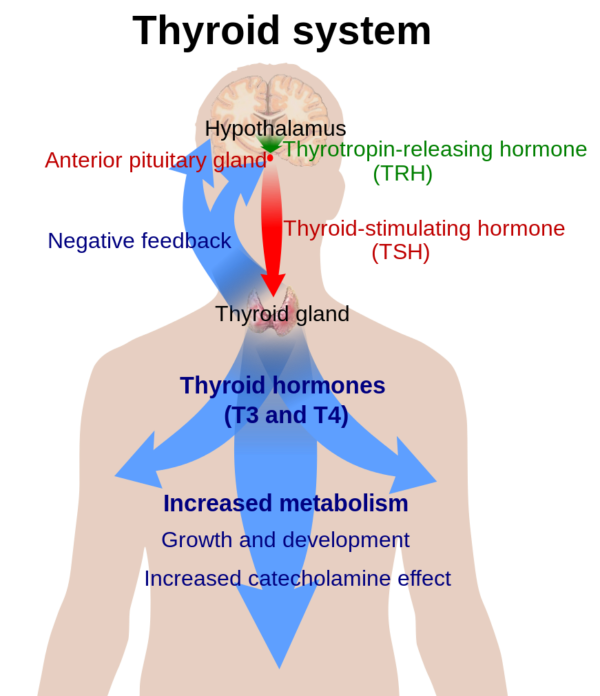
The hypothalamus-pituitary-thyroid feedback loop is a negative feedback process that regulates synthesis and release of thyroid hormone from the gland. The simplest view of thyroid hormone feedback is presented in this image.
Elevated plasma T3 and T4 has a negative effect at the pituitary and at the hypothalamus of the brain, which slows the synthesis and release of thyroid releasing hormone (TRH) from the hypothalamus and thyroid stimulating hormone (TSH) from the pituitary. With less TSH in the blood the gland synthesizes less T3 and T4.
However, the system is more complex than it first appeared. Multiple other factors in addition to a drop in TRH secretion slow the synthesis and release of TSH.
Somatostatin and dopamine, brain neurotransmitters, and glucocorticoid from the adrenal gland inhibit synthesis and release of TSH. Also, several pituitary peptides affect TSH production and release.
In fact, there is a daily rhythm of TSH in blood. Plasma TSH is low during the day and increases in early evening, peaking near the beginning of sleep. This hormonal rhythm is generated by the part of the hypothalamus known as the biologic clock of the brain. Neurons of the clock region synapse on the TRH neurons in another part of the hypothalamus.
Multiple neuron pathways in the brain also connect to the thyroid gland indirectly through the autonomic nervous system. Fasting disconnects the basal negative feedback loop. It decreases T3 and T4 in plasma while TSH either remains the same or falls. One theory is that this is a way to conserve energy when food is short.
5 Tips for learning the endocrine system
Thyroid hormone and parathyroid hormone regulation represent two of the simpler endocrine feedback systems in the body. That is why I chose them for this and my last post. However, they do illustrate general features found in endocrinology. Here are the elements to look for when learning the endocrine system.
- Cells with components necessary to synthesize and secrete hormone into blood
- Cells with protein receptors that bind a hormone found in blood
- Receptor binding that sets in motion cellular pathways
- Brain neurons that respond to hormone level fluctuation in blood
- A negative feedback regulatory loop – positive feedback exists, but is rarely used
Further reading:
Hormone Regulation of Plasma Calcium: Human
Do you have questions?
Send me an email with your questions at DrReece@MedicalScienceNavigator.com or put them in the comment box. I always read my mail and answer it. Please share this article with your fellow students taking anatomy and physiology by clicking your favorite social media button.
Margaret Thompson Reece PhD, physiologist, former Senior Scientist and Laboratory Director at academic medical centers in California, New York and Massachusetts is now Manager at Reece Biomedical Consulting LLC.
She taught physiology for over 30 years to undergraduate and graduate students, at two- and four-year colleges, in the classroom and in the research laboratory. Her books “Physiology: Custom-Designed Chemistry”, “Inside the Closed World of the Brain”, and her online course “30-Day Challenge: Craft Your Plan for Learning Physiology”, and “Busy Student’s Anatomy & Physiology Study Journal” are created for those planning a career in healthcare. More about her books is available at https://www.amazon.com/author/margaretreece. You may contact Dr. Reece at DrReece@MedicalScienceNavigator.com, or on LinkedIn.
Dr. Reece offers a free 30 minute “how-to-get-started” phone conference to students struggling with human anatomy and physiology. Schedule an appointment by email at DrReece@MedicalScienceNavigator.com.


Comments
Thyroid Hormone: What Does It Do? — No Comments
HTML tags allowed in your comment: <a href="" title=""> <abbr title=""> <acronym title=""> <b> <blockquote cite=""> <cite> <code> <del datetime=""> <em> <i> <q cite=""> <s> <strike> <strong>